We use cookies on this site to improve our service, perform analytics, and remember website preferences. By using this site, you consent to these cookies. For more information visit our Privacy Policy
Applying human factors to digitizing critical hospital workflows
The Massive Hemorrhage Protocol (MHP) at an institution dictates procedures when a patient is experiencing massive blood loss at an incredible rate. When University Health Network (UHN) wanted to transition their MHP workflow to a fully-digitized system, HHF was tasked with conducting current state research and usability testing to ensure that this could be done without compromising patient safety.
Client
University Health Network (UHN)
Services
Clinical Observations, Ethnographic Research, Usability Testing
Challenge
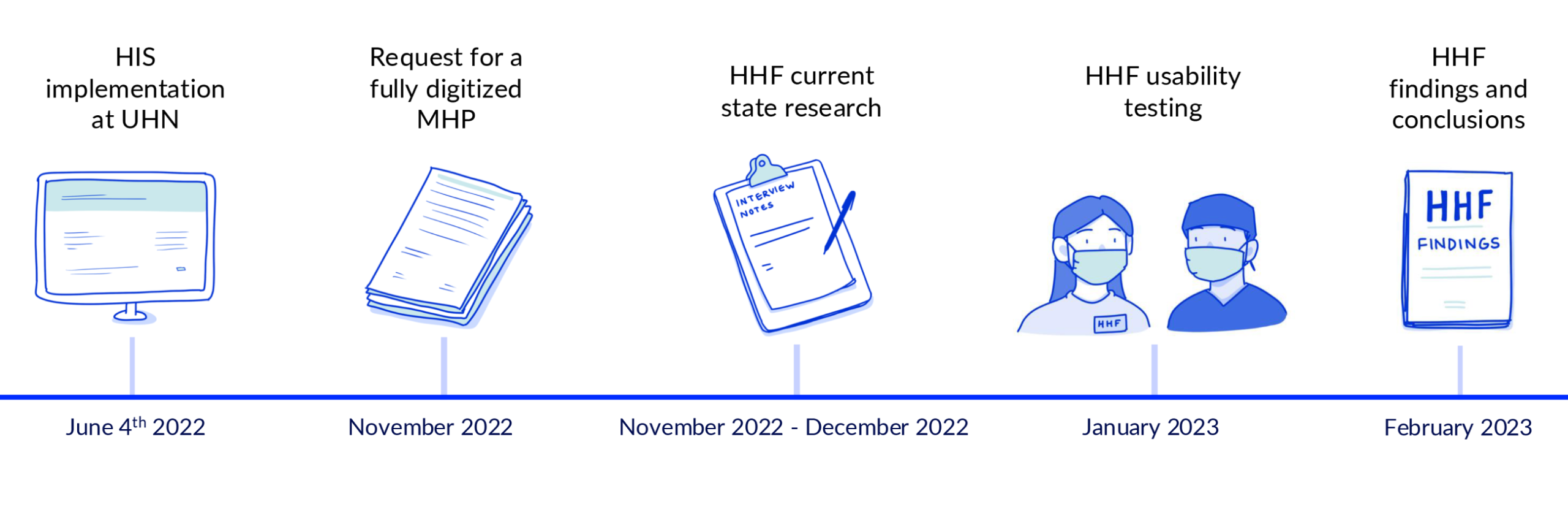
University Health Network (UHN) in Toronto launched the implementation of a new health information system on June 4th, 2022. The shift to a singular digital system from the decades-long reliance on complex paper-based and hybrid-digital workflows aimed to enhance healthcare delivery for both patients and providers. The Massive Hemorrhage Protocol (MHP) is an example of UHN’s use of a paper-based system, particularly in a high-risk and increased criticality clinical environment. The MHP did not undergo a complete digital transformation during the implementation at UHN but was instead transitioned into a hybrid workflow consisting of both paperwork and digital input tasks. It remained hybrid until later in 2022 when UHN sought to adopt a digital MHP, requiring a fully electronic workflow that retained the fundamentals of the paper-based system. This digital workflow had the potential to provide a singular system when engaging the MHP, which could improve healthcare experiences for countless patients and providers. However, before launching this digital workflow, HHF was tasked with determining if it would be a safe solution.
Process
Discovery
The Massive Hemorrhage Protocol is the procedure that an institution follows when the provision of large quantities of blood (or blood products) is needed for a rapidly hemorrhaging patient. This is a highly critical, high risk, and urgent situation, that cannot operate under the wait time of a typical blood order. MHP involves the collaboration of different moving parts and stakeholders, including doctors, nurses, code responders, and blood bank technicians.
To assess how a digitized MHP compares to the current hybrid approach, HHF had to develop a firm understanding of the current state. This consisted of a series of observations, shadowing clinical units, and conducting staff interviews. As HHF is located directly within UHN, our usability experts had the opportunity to speak directly with clinicians who are well versed in the MHP and observe their procedures. HHF gathered data on response times, unit structure, and other feedback directly from clinicians who use the MHP on a regular basis.
Testing
With a firm understanding of how the MHP is used in practice, HHF used this information to develop a plan for testing the newly digitized approach that would be representative of real workflows. HHF conducted two separate usability studies: one focusing on physicians and nurses and another focusing solely on blood bank technicians. These tests were held in HHF’s simulation labs, adapted to match the inpatient units and blood bank workstations HHF had observed. Participants in these studies conducted blood and blood product ordering tasks, much like they would in practice – but now using the digital implementation.
While users performed tasks, HHF usability experts worked to identify any use issues experienced by the participants and their root causes. The HHF team identified a wide range of issues users experienced or were concerned by, including the following:
- Users sometimes ordered too little blood by mistake.
- Users did not realize when blood orders had not been released, leaving the ordering process incomplete.
- Tasks that used to happen in tandem now had to be done sequentially on a digital system, which slowed things down.
- The digital system could only be used where computers were available, which had been a less prevalent limitation in a hybrid approach.
- The proposed digital workflow meant that staff would spend more time on the computer and less time caring for the patient in a critical emergency.
Outcomes
After gathering all use issues identified through usability testing, HHF provided a detailed report to UHN outlining all findings and their impacts on clinical workflows and patient safety. Many of the use issues observed were likely to result in inadequate patient care, a delay in the blood ordering process, and patient safety events. After taking into consideration the concerns identified by HHF, the UHN steering committee ultimately decided not to move forward with the digital solution and instead maintained the hybrid approach.
When hospitals make big changes to workflows, especially for emergency processes, it’s important to test how those changes will affect real people. It remains more important than ever to consider human factors in the implementation of new systems or procedures to keep patient safety at the forefront. Taking the time to perform usability testing and human factors analyses on new systems can gather critical information. At HHF we will continue to take a proactive approach to identifying usability concerns before they ever have the chance to become patient safety events.
HHF’s labs were converted into a representative setting for the MHP scenario.